(TX_RTT) Number of ART patients with no clinical contact (or ARV drug pick-up) for greater than 28 days since their last expected contact who restarted ARVs within the reporting period
Export Indicator
TX_RTT counts those who are lost to TX_CURR for more than 28 days past the last expected clinical contact and who return to care and restart ARVs in the reporting period. Monitoring this indicator may also help to identify those PLHIV who were diagnosed and started ART in the past but have been lost to the health care system.
This indicator seeks to encourage ongoing contact with patients who miss appointments and/or to encourage supportive services to facilitate restarting ARV therapy. It also seeks to encourage identification and the return to treatment of those PLHIV with a history of ART but are currently lost or unknown to the health care system.
National clinical guidelines typically recommend that patients with ART history are restarted on ARVs, rather than newly initiate clients as if they were treatment-naïve. Nonetheless, many clinics – lacking sufficient clinical history or documentation – newly initiate patients with prior ART history.
From a public health perspective, treatment adherence and retention are essential to achieve and maintain viral suppression and ultimately reduce or eliminate disease transmission. Serious attempts should be made to reengage and return to treatment any patient that has not returned for clinical services or drug pick-up.
Number of ART patients with no clinical contact or ARV pick-up for greater than 28 days since their last expected contact who restarted ARVs within the reporting period
N/A
How to calculate annual total: Data for this indicator can be summed across reporting periods
How to collect:
When a patient has missed their most recent expected clinical contact, the clinic or other related staff should attempt to reach and reengage the patient as soon as possible.
A patient is counted under TX_RTT in the reporting period in which s/he returns to care and restarts ARVs. As with TX_NEW, the TX_RTT patient joins the TX_CURR population; if the patient remains on ART to the end of the reporting period, the patient should be counted as TX_CURR in that reporting period.
A patient should not to be counted as TX_RTT if they have been traced and returned to treatment within 28 days of the last expected contact (clinical or ARV pick up).
Clinical contact is defined as reporting to the clinic for ART pick-up or clinical assessment, or a documented community visit with a community health worker or peer from an ART refill group.
Key Populations (KPs):
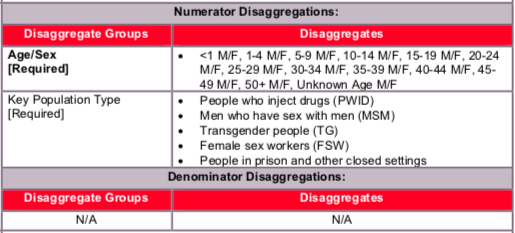
Both KP-specific and clinical partners should complete these KP disaggregations, but only if safe to maintain these files and to report. Reporting of the key population disaggregation should be consistent with what is described under the KP_PREV “How to review for data quality” section on mutual exclusivity of an individual who falls under multiple KP categories (e.g., FSW who injects drugs). In such instances, the individual should only be reported in ONE KP disaggregation category with which this person is most identified. See Appendix A to support the identification of key populations at service delivery.
The first priority of data collection and reporting of treatment among key populations must be to do no harm. These data must be managed confidentially to ensure the identities of individuals are protected and to prevent further stigma and discrimination of key populations.
How to review for data quality: Confirm that TX_CURR ≥ TX_RTT
Reporting level: Facility
Reporting frequency: Quarterly
These are previously ART experienced individuals who reinitiate ARVs after being off treatment for ≥28 days (and therefore LTFU).
Indicator changes (MER 2.0 v2.3 to v2.4): New indicator
PEPFAR-support definition:
Standard definition of DSD and TA-SDI used.
Provision of key staff or commodities for PLHIV receiving ART include: the provision of key staff and/or commodities can include ongoing procurement of critical commodities, such as ARVs, or funding for salaries of HCW who deliver HIV treatment services. Staff who are responsible for the completeness and quality of routine patient records (paper or electronic) can be counted here; however, staff who exclusively fulfill MOH and donor reporting requirements cannot be counted.
Ongoing support for PLHIV receiving ART service delivery improvement includes: clinical mentoring and supportive supervision of staff at HIV sites providing ART, support for quality improvement activities, patient tracking system support, routine support of ART M&E and reporting, commodities consumption forecasting and supply management.
Guiding narrative questions:
- How long were people off of ARV? What percentage of PLHIV returned to care were off ARVs for 12 months or more? What interventions supported their return to care?
- What portion of an increase in TX_CURR is attributable to TX_RTT (vs. TX_NEW) in the reporting period?
- Taken together, what does TX_NEW, TX_ML, TX_CURR, TX_NET_NEW, and TX_PVLS tell you about the quality of the treatment program at the facility?