(TX_ML) Number of ART patients (who were on ART at the beginning of the quarterly reporting period) and then had no clinical contact since their last expected contact
Export Indicator
TX_ML (treatment mortality and lost to follow up) is intended to: (1) help better understand fluctuations or steady growth in TX_CURR over time, (2) encourage tracing of patients when a patient has had no clinical contact for greater than 28 days since their last expected contact and (3) promote timely identification of patient outcomes among patients known to have missed clinical visits or drug pickups. PEPFAR implementing partners must ensure that immediate programmatic action is being taken to locate patients that have had no clinical contact for greater than 28 days since their last expected clinical contact. Serious and repeated attempts should be made to reengage any such patients and return them to treatment. In case of death, mortality data should be analyzed and investigated to determine causes of death, where possible.
From a public health perspective, treatment adherence and retention are essential to achieve and maintain viral suppression and ultimately reduce or eliminate disease transmission. Not uncommonly, patients who are lost-to-follow up, may have died or have self-transferred to another health care facility; as such, it is important to understand and make these distinctions as each one may require different programmatic interventions.
Serious attempts should be made to reengage any patient that has not returned for clinical services or drug pick-up and return them to treatment, and mortality data should be analyzed and investigated to determine causes of death amenable to programmatic intervention (e.g., TB, opportunistic infection, cervical cancer).
It is important to note that this is not a cohort monitoring indicator. TX_ML is meant to be used in conjunction with TX_CURR to help better understand fluctuations or steady growth of the ART patient population.
Number of ART patients with no clinical contact or ARV pick-up for greater than 28 days since their last expected clinical contact or ARV pick-up
N/A
How to calculate annual total:
There should be no annual total. Data for this indicator are intended to provide context for TX_CURR results but the numerator should NOT be summed across reporting periods due to the active movement and potential reclassification of patients.
How to collect:
When a patient has missed their most recent expected clinical contact, the clinic or other related staff should attempt to reach and reengage the patient as soon as possible. Once a PLHIV has reached 28 days past their expected clinical contact or drug pick-up, s/he should be removed from TX_CURR, the clinic should again attempt to reach and re-engage the patient, and his/her current outcome should be determined. The outcomes are defined as not currently on ART at the facility if the patient:
- Died
- Lost to follow up
- On treatment for <3 months when LTFU
- On treatment for >3 months when LTFU
- Transferred out
- Refused/stopped treatment
See Disaggregates and Descriptions section below for definitions of each of these outcomes.
If the patient is re-engaged and restarted ART after >28 days of being off treatment, then the patient should be counted in TX_RTT in the reporting period and added back to TX_CURR, but should not be counted in TX_ML.
Included in the classification of LTFU are the following: patients for whom tracing is not attempted, and patients for whom tracing is attempted but unsuccessful or for whom status cannot otherwise be determined (i.e., patient may have died or may have silently transferred, but status is unknown). A facility may wish to further distinguish these classifications, but they are not required for MER reporting. It is assumed that tracing will be attempted for every patient who has missed clinical visits at both <28 days and >28 days since the last expected clinical contact or ARV pick-up.
This indicator seeks to reconcile the status of patients who are TX_CURR during the reporting period and then fall off of ART, i.e., into the classification of >28 day since clinical contact or ARV pick-up status DURING THE REPORTING PERIOD. This includes those ART patients who continue treatment from the prior reporting period (TX_CURR at the beginning of the reporting period), those who newly initiate in this reporting period (TX_NEW), and those who return to care or restart in this reporting period (TX_RTT). To reiterate, this indicator should not count or report those patients who were already lost and not counted in TX_CURR at the beginning of the reporting period.
Facilities should make every attempt to continue to contact persons LTFU from a prior reporting period and return them to care, an outcome which would be reflected in the TX_RTT indicator.
It is widely acknowledged that even where reporting is required, mortality data, especially cause of death, are often underreported or inaccurate. In addition, it may take some time for a clinic to discover that a patient has died. Thus, a clinic may classify a patient as TX_ML_LTFU in the quarter the patient gets to >28 days past the expected clinical contact, but later discover that the patient died. If it is later discovered that the patient died, they do not need to be recounted or reclassified in this indicator in a later quarter. Data on deaths should only be reported, if available, in the quarter when the patient gets to >28 days past the expected clinical contact.
Program data available on deaths and the cause of death disaggregate under this indicator should be triangulated with mortality surveillance, where available, to understand causes of death among PLHIV. For more information on routine mortality monitoring, refer to Appendix H.
How to review for data quality:
Patient trackers, tracing logs, missed appointment reports, and other available sources should be routinely checked. These comparisons will help programs understand where efforts are required to better improve and/or ensure completeness of reporting.
Reporting level: Facility
Reporting frequency: Quarterly
![]()
![]()
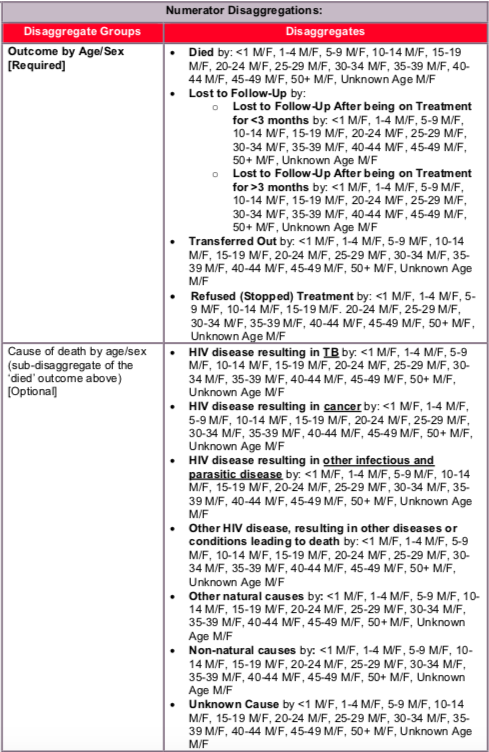
Disaggregate descriptions and definitions:
Outcome definitions:
- Died: Patient was confirmed as dead by direct observation or by unambiguous report of family or close contact (neighbors, co-workers, etc.); it should not be presumed.
- Lost to follow-up: Patient status has not or cannot be assessed (did not attempt to trace or traced but unable to locate). Regardless of whether the patient was on treatment for <3 months or greater than 3 months, LTFU is defined as:
- Traced patient (unable to locate): Exhaustive attempts (e.g., phone calls, home visits, triangulation with other health facilities) were made to locate the patient, but patient was still not located through these efforts. Exhaustive attempts means completing more than 3 attempts to contact or locate the patient using multiple methods.
- Did not attempt to trace patient: No attempt was made to trace the patient during the reporting period.
- Transferred out: Patient was confirmed to be successfully transferred to another health facility during the reporting period, this includes both “silent transfers” and “down-referrals.” A ‘down-referral’ refers to those instances where a patient is initiated at one facility (counted as TX_NEW and possibly TX_CURR at the initiating facility) and then transferred to a lower level facility for ongoing ART. “Silent transfer” refers to those clients that are lost to treatment at one facility, but have re- entered treatment at another facility without notifying the original departing facility. Through active tracing, the originating facility may learn that a patient has silently transferred.
- Refused (Stopped) ART: Patient was contacted and confirmed to have stopped ART during this reporting period. Reasons that the patient stopped ART should be investigated and well documented in the narratives for this indicator (e.g., stigma and discrimination, faith healing, etc.).
This indicator was originally introduced in FY19 and marked the first time PEPFAR collected mortality information through routine program data. Mortality is an essential measure to assess the impact of the health sector more broadly, and the HIV program in particular. Mortality data should be compared between sites and districts as well as by age and sex to determine the geographic and demographic areas where intensified interventions are most needed. Particularly, determining the cause-of-death (COD) or conditions experienced at the time of death among PLHIV can be used to help identify programmatic gaps and focus resources on interventions aimed at reducing preventable deaths.
Appendix I describes the ICD codes associated with the cause of death categories outlined below.
Cause of death definitions:
- HIV disease resulting in TB: Any patient with known or presumed TB (pulmonary and/or extra-pulmonary) at the time of death without another identified COD
- HIV disease resulting in other infectious and parasitic disease: Any patient who died from any infectious cause other than TB; this includes infections not otherwise specified
- HIV disease resulting in cancer: Any patient with known or presumed cancer at the time of death
- Other HIV disease, resulting in other diseases or conditions leading to death: Any patient who died from a non-infectious, non-malignant cause that was related to HIV, such as acute HIV infection syndrome, (persistent) generalized lymphadenopathy, hematological and immunological abnormalities, etc.
- Other natural causes: Any patient who died from natural causes (including certain cancers and infections, etc.) that were not directly related to HIV disease.
- Non-natural causes: Any patient who died from non-natural causes (e.g., trauma, accident, suicide, war, etc.)
- Unknown cause: Patients in whom cause of death was truly not known
Clinical contact is defined as any clinical interaction with the patient, such as clinical assessment by a healthcare worker or provision of medication.
Indicator changes (MER 2.0 v2.3 to v2.4):
- Reporting frequency changed to quarterly to align the reporting of this indicator with other core HIV clinical cascade indicators.
- Outcome disaggregations simplified to the following categories: died, lost to follow-up (LTFU), transferred out, and refused (stopped) treatment.
- Sub-disaggregation added to the LTFU outcome for patients LTFU after being on treatment for >3 months vs. patients LTFU after being on treatment <3 months. This distinction was added to highlight the critical nature of early retention for successful longer-term retention among those persons newly initiating ART, especially otherwise healthy or younger adults.
PEPFAR-support definition:
Standard definition of DSD and TA-SDI used.
Provision of key staff or commodities for PLHIV receiving ART include: the provision of key staff and/or commodities can include ongoing procurement of critical commodities, such as ARVs, or funding for salaries of HCW who deliver HIV treatment services. Staff who are responsible for the completeness and quality of routine patient records (paper or electronic) can be counted here; however, staff who exclusively fulfill MOH and donor reporting requirements cannot be counted.
Ongoing support for PLHIV receiving ART service delivery improvement includes: clinical mentoring and supportive supervision of staff at HIV sites providing ART, support for quality improvement activities, patient tracking system support, routine support of ART M&E and reporting, commodities consumption forecasting and supply management.
Guiding narrative questions:
- Describe patient tracing efforts in more detail. When does patient tracing occur (e.g., within 1 week of missed contact, within 4 weeks of missed contact, etc.)?
- For all clients that refused (stopped ART), what reasons were cited for refusal [e.g., discrimination by the health facility, unfriendly services, inconvenient services (e.g., long wait times, asked to come back too frequently), faith healing, etc.]? How is the partner or country team working to address these issues and reengage these clients on life-saving ART?
- What percentage of LTFU patients (patients with no clinical contact for ≥ 28 days) received an active follow-up visit during the reporting period?
- What is being done to address facilities with above average mortality? Or a higher than average number of patients who were untraceable?
Related Indicators
AV.2 Total attrition from ART, 2020, WHO Consolidated HIV strategic information guidelines: driving impact through programme monitoring and management (https://www.who.int/publications/i/item/consolidated-hiv-strategic-information-guidelines).