(PP_PREV) Number of priority populations (PP) reached with the standardized, evidence-based intervention(s) required that are designed to promote the adoption of HIV prevention behaviors and service uptake
Export Indicator
The indicator represents PEPFAR-supported programming only and helps to determine PEPFAR’s reach to priority populations. It may also help inform coverage of PEPFAR-supported programming for priority populations when reliable population size estimates are available.
Priority populations: Priority populations should be defined by each country in the indicator narrative and must have a documented HIV prevalence or incidence greater than the general population of the country. Groups that might be counted as priority populations include:
- Adolescent girls and young women (determined using the reported age/sex disaggregations)
- Adolescent boys and young men (determined using the reported age/sex disaggregations)
- Adult men women (determined using the reported age/sex disaggregations)
- Clients of sex workers
- Displaced persons
- Fishing Communities
- Military and other uniformed services
- Mobile Populations
- Non-injecting drug users
Package of interventions: Together with the IP, the country team designs a set of interventions for each of the priority populations. In a defined catchment area for the specific priority population, all prevention interventions may not be offered by one IP. However, all required intervention must be available in the catchment area for the priority population. Interventions must adhere to written protocols, include goals and activities, and be designed to promote adoption of key behaviors that support HIV prevention and service uptake among the priority population(s). The interventions should comprise multiple encounters with the same individuals or groups.
Children aged 9-14 who are receiving an approved primary prevention of HIV and sexual violence intervention should be reported under OVC_SERV and not PP_PREV. Please see the OVC_SERV reference sheet for further detail.
HIV testing services (HTS) or referring an individual to HTS is required to be offered (at least once during the reporting period and/or in accordance with WHO/national guidance) unless the individual had previously been tested positive for HIV. If the individual is self-identified as HIV positive, then HTS provision or referral to HTS will not be a required element of this indicator.
Conducting risk assessments or screening to determine the need for HIV testing also meets the HTS component of PP_PREV. For example, if there is a ten-year-old girl enrolled in DREAMS, we would anticipate that she would not need to be tested for HIV if a risk assessment determines that she is not sexually active, and she does not have any additional risk factors for HIV.
The table below lists the interventions that must be offered in addition to HTS (or HTS screening/referral).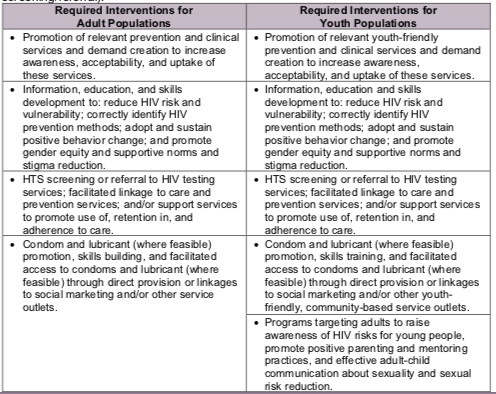
Number of priority populations reached with standardized HIV prevention intervention(s) that are evidence-based
N/A
How to calculate annual total:
Sum across both reporting periods; de-duplicating unique individuals already reached and reported in Q1-Q2 of the same fiscal year in Q4 reporting.
How to collect:
Data collection requires reliable tracking systems that are designed to count the number of one-on-one encounters or participation in group interventions and that reduce double-counting of individuals in a reporting period. Data should be collected at every encounter/point of service and aggregated in time for PEPFAR reporting cycles. This indicator only counts those interventions at the individual and/or group level.
A partner may count an individual (with unknown HIV sero-status or self-identified as HIV negative) as having received a prevention intervention if they have provided HTS and/or referral to HTS AND at least one of the other listed prevention interventions during the reporting period. If an individual is already known to be HIV positive at the time of service delivery, s/he should receive at least one of the interventions listed in the table (outside of HTS) to qualify as being counted under this indicator.
Tracking systems must be able to reduce double-counting of individuals in a reporting period. An individual will be reported when he/she first receives any of the required interventions in the reporting period; if the same individual receives any subsequent interventions during the same reporting period they will be reported as a returning beneficiary and not counted again in the reporting period.
Furthermore, de-duplication of all returning beneficiaries within the Q3-Q4 reporting period (April 1 – September 30) will also need to take place in Q4 reporting if they had already been counted under PP_PREV in Q1-Q2 of the same fiscal year. For example, if an individual had received prevention interventions under PP_PREV through PEPFAR-supported program in January 2017 and was counted as being reached in FY17 Q2 reporting cycle, and this same individual was later reached with prevention services again by PEPFAR-supported program in June 2017, that individual should NOT be reported again in the FY17 Q4 reporting period. This de-duplication is critical to accurately track the ANNUAL number of unique individuals reached by PEPFAR within a given fiscal year. Trend analysis of past performance PP_PREV data will be adversely affected with the change in frequency of PP_PREV reporting from annually to semi-annually if this de-duplication is ignored (i.e., annual number of PP_PREV reported within the same fiscal year would be inflated as the same individual would be counted twice if this de-duplication does not occur at Q4 reporting).
If possible, a unique identifier should be assigned to program participants or names can be collected to track individual participation in the prevention interventions/sites.
Site (facility and community) level system should maintain accurate registers for each individual priority population and sum these individual populations when reporting this indicator.
How to review for data quality:
Data should be reviewed regularly for the purposes of program management, to monitor progress towards achieving targets, and to identify and correct any data quality issues.
Testing services disaggregates should not exceed the numerator.
Reporting level: Facility & Community
Reporting frequency: Semi-Annually
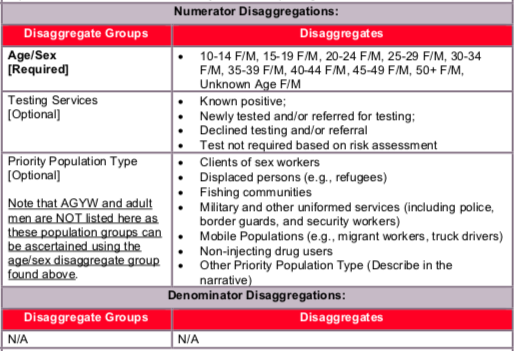
Testing Services Disaggregates Definitions:
- Known Positive: Persons within each key population type for whom HIV testing is not indicated because they are known to be HIV-positive. HIV-positive test results should be verified, if possible, for all persons accessing HIV prevention services during the reporting period. Implementing partners should maintain records (without personally identifiable information) on whether the HIV-positive client is linked to treatment. Patients tested positive in previous reporting periods should be counted as Known Positives.
- Newly Tested and/or Referred for Testing: Persons within each key population type for whom HIV testing is indicated because they do not know their HIV status or their last HIV-negative test was more than 3-6 months ago (or more/less frequently as indicated by National Guidelines) should either be offered an HIV test on site or given information about where and when they can access an HIV test at another nearby clinic. Every attempt should be made to ensure the client is linked with HIV testing services that are PP-friendly, and where possible the completed referral should be documented (i.e., the client accessed HIV testing). Note: Persons who access testing and whose results are newly tested HIV-positive in the reporting period should also be counted under “newly tested” even if they return for additional prevention services during that reporting period.
- Declined Testing and/or Referral: Persons who, after explaining the benefits of HIV testing and the reason for testing every 3-6 months (or more/less frequently as indicated by National Guidelines), decline to be tested on-site or referred to a site where HIV testing is offered. Although every attempt should be made to support key populations with HIV testing as part of the package of HIV prevention services and to provide HIV testing on site or PP-friendly sites, programs should also respect the autonomy of clients to decline this service. Clients who decline testing and/or referral can still receive other prevention services, as long as the benefits of HIV testing were explained and testing or a referral for testing was offered.
- Test not required based on risk assessment: Persons who, based on screening or a risk assessment, do not require a test for HIV during the reporting period. That is, it was determined through the screening or risk assessment that an HIV test was not needed.
The numerator is the number of individuals from each priority population reached with HIV prevention interventions during the reporting period. For the purposes of reporting, the team will sum the numbers reached in each of the priority populations and report that total (details of the priority populations reached should be explained in the narratives).
Indicator changes (MER 2.0 v2.3 to v2.4):
- New disaggregate added to the “Testing Services” disaggregate group for “Test not required based on risk assessment” for those priority populations not eligible for HTS based on HTS screening.
In-text clarifications added to confirm that conducting HIV risk assessments meets the required HTS component for PP_PREV.
PEPFAR Support definition:
Standard definition of DSD and TA-SDI used.
Provision of key staff or commodities for priority populations receiving HIV prevention services includes: ongoing procurement of critical commodities such as condoms, teaching materials, or community promotion materials; funding for salaries of personnel who deliver components of the intervention; or paying for transportation of those staff to the point of Service delivery. Staff responsible for the completeness and quality of routine patient records (paper or electronic) can be counted here; however, staff who exclusively fulfill MOH and donor reporting requirements cannot be counted.
For priority populations receiving HIV prevention, ongoing support services service delivery improvement includes: site supervision; training or assistance with monitoring and evaluation; QI/QC; and development of materials and protocols.
Guiding narrative questions:
- Please help us understand what is being tracked or counted under PP_PREV:
- Describe the types of activities or interventions that are being provided to beneficiaries.
- If a specific evidence-based intervention or curriculum is being implemented, please provide the name.
- Specify the priority populations counted under PP_PREV and if priority populations are either receiving the intervention themselves or indirectly benefiting from intervention, based on other beneficiaries’ receipt or access to the intervention.
- PP_PREV requires that “HIV testing services (HTS) or referring an individual to HTS (at least once during the reporting period) unless the individual self-identifies as HIV positive.
- Are you tracking the number of HTS referrals generated through PP_PREV activities? If so, please provide the number.
- If you are not tracking the HTS referrals please state so and provide an approximation.
- If PP_PREV increased or decreased by >25% since the last reporting period, please explain the reasons (e.g., budget changes, changes to how curriculum-based interventions are tracked, activities included in PP_PREV that were previously counted elsewhere, etc.).