People living with HIV who have suppressed viral loads
Export Indicator
Individual-level viral load is the recommended measure of antiretroviral therapy efficacy and indicates treatment adherence and the risk of transmitting HIV. A viral load threshold of <1000 copies/mL defines treatment success according to the 2016 World Health Organization (WHO) Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. People with viral load test results below the threshold should be considered as having suppressed viral loads.
Viral suppression among people living with HIV provides a benchmark for monitoring global targets over time and a standardized indicator of HIV treatment and prevention success, critical to ending the AIDS epidemic. When considered as a proportion of the number of people on treatment (the numerator of Indicator 2.2), this indicator monitors the third 95 of the UNAIDS 95-95-95 targets: that 95% of the people receiving antiretroviral therapy will have suppressed viral loads by 2025.
Number of people living with HIV in the reporting period with suppressed viral loads (<1000 copies/mL)
Estimated number of people living with HIV (to estimate viral load suppression coverage);
OR
Estimated number of people living with HIV who are on treatment (to determine progress towards the third 95).
Numerator/denominator
Note: Countries with a population of more than 250 000 will report on this indicator by broad age groups, in the Spectrum HIV estimates file. Results will be obtained directly from the final national Spectrum file, alongside all other Spectrum-estimated indicators. Reporting on sub-national data for the indicator will be done in the Global AIDS Monitoring reporting tool. If a country has sub-national estimates developed using Naomi, these data will be obtained directly from the final Naomi file.
Viral suppression is defined as <1000 copies/mL. Some countries use other thresholds (such as undetectable, <50 copies/mL or <400 copies/mL), and require adjustment for comparability with other countries and for monitoring the global 95-95-95 target. UNAIDS recommends that countries adjust for lower threshold detection This is done using the formula:
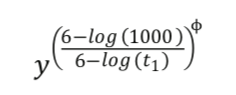
In this instance, y is the standard (1000 copies /mL) viral suppression level, t1, is the country's alternative threshold that was used, and ɸ is the region-specific adjustment factor. This adjustment will be done automatically in Spectrum, if required.
Viral load suppression may be reported from three data sources: (1) clinical and programme data; (2) nationally representative surveys (such as the Population-based HIV Impact Assessment [PHIA] and HIV drug resistance surveys); or (3) early warning indicators of HIV drug resistance surveys. Countries should report data from whichever source is most recent and nationally representative.
- Routine viral load suppression tests from people on antiretroviral treatment collected through clinical or laboratory registers or case surveillance
For the numerator. Countries should report the estimated number of people nationally who have suppressed viral loads during the reporting period if viral load testing coverage (i.e., the number of people routinely tested during the reporting period, as per WHO guidance, among all people on treatment) is 50% or greater.
Countries that report viral load testing coverage of less than 50%, should, in contrast, only report the number of routine viral load tests - but not the number where the viral load is below the threshold, because this then is not a good, representative estimate for the overall population on treatment. Countries still wishing to use viral load result data despite viral load testing coverage below 50% should discuss with UNAIDS, to determine whether the percentage of people suppressed in the tested population can be considered representative for the population on ART with no access to testing.
Countries should only include testing data that result from routine testing among those on treatment, and not targeted testing to a select subgroup of patients on treatment. For example, a person's results should not be included if testing was done prior to treatment initiation or for the reason of a suspected treatment failure. If viral load is tested repeatedly for a person within the year, only the last routine test result should be used.
For countries where annual viral load testing coverage is 50% or over, an estimated number of people with suppressed viral loads should be reported. This is calculated from the number suppressed among those tested, multiplied by the total number of people on treatment. This assumes that levels of suppression in the untested population are the same as those in the tested population. This assumption is supported by evidence from South Africa, which shows that although viral load information was frequently missing, estimates of viral suppression did not change substantially after adjusting for missing data.
Example: A country with an estimate of 100 000 people living with HIV has routine viral load tests for 12 000 of the 24 000 people receiving antiretroviral therapy. The viral load testing coverage is 50%, and the country deems the level of viral load suppression in the untested population to be like that among the tested population of people on treatment. Of the 12 000 people tested, 10 000 people have suppressed viral loads. The estimated national number of people living with HIV who have suppressed viral loads is 20 000 [(10 000/12 000) x 24 000].
Where viral load suppression in the untested population on treatment is likely to not equal that in the tested population, please contact UNAIDS for further discussion about approaches for estimating this count.
For the denominator. Estimation models such as Spectrum are the preferred source for the number of people living with HIV. UNAIDS will work with countries to develop a Spectrum model that matches the estimate of people living with HIV if national estimates other than those produced through Spectrum are used.
For more information on estimating the number of people living with HIV who are on treatment, as part of calculating the third 95, please see Indicator 2.2.
- Recent nationally representative population surveys (including household, acquired HIV drug resistance surveys or early warning indicators (EWI) survey of HIV drug resistance)
For the numerator. The proportion reported to have suppressed viral loads among people testing positive in the survey should be multiplied by the total number of people estimated to be living with HIV nationally to obtain the total number of people who have a suppressed viral load. This value may slightly overstate the number of people who are virally suppressed among those on treatment, since it will include some people who are not on treatment but naturally suppress the virus. If using data from an acquired HIV drug resistance survey, either the 12- or 48-month cohort data may be used. Data from early warning indicators should only be used to generate national aggregate statistics if:
a) all clinics in a country - or a random sampling of clinics - reported early warning indicators data that includes at least 70% of all people on ART from the sampled clinics.
OR
b) if convenience sampling of clinics was used, a national aggregate statistic can be reported if the data from the sampled clinics includes at least 70% of the eligible population on ART in the country (see page 8 of the Early Warning Indicators (EWI) annex - sampling guidance - see References below).
Note: Countries using survey data should still report on the number of people on treatment with routine viral load tests during the reporting period. Survey data should only be used if conducted in both children and adults.
For the denominator. Estimation models such as Spectrum are the preferred source for the number of people living with HIV. UNAIDS will work with countries to develop a Spectrum model that matches the estimate of people living with HIV if estimates other than those produced through Spectrum are used. For more information on estimating the number of people living with HIV who are on treatment as part of calculating the third 95 target, please see Indicator 2.2.
Annually
- 0–14 years for children and 15 years and older by sex (men and women) for adults; data reported for unknown age or sex should be allocated to the age and sex disaggregated data cells using the same distribution of the data with known age and sex. These adjustments should be noted in the box providing additional information.
- As available. Disaggregation by detailed age and sex: <1 year, 1–4 years, 5–9 years and 10–14 years for children and 15–19 years, 20–24 years, 25–49 years and 50+ years by sex (men and women) for adults; by gender (men, women, other gender) for adults.
If there are subnational data available, please provide the disaggregation by administrative area, city, or site in the space provided.
When viral load suppression testing data are collected from all people receiving antiretroviral therapy or a nationally representative sample, this measurement provides important information on adherence, treatment efficacy and transmission risk at the individual and programme levels. Despite the indicator’s importance, several challenges may arise in accurately monitoring it using currently available programme data. First, because viral load monitoring capacity is being scaled up but remains limited in low-income settings, estimates of viral load suppression in the tested population may not be representative of the untested population when measured through programme data. This is especially the case if scale-up of testing is biased to higher or lower performing sites. By assuming that the levels of viral load suppression are the same in the tested and untested population when testing coverage is not complete, progress toward the 95–95–95 targets may be under- or overstated.
A second challenge arising from the currently available programme data is that viral load testing may be performed selectively to confirm suspected treatment failures. The data reported from the viral load testing of people suspected of treatment failure will underestimate population-level viral load suppression. UNAIDS recommends that countries closely review reported data to exclude targeted, non-routine testing.
A third challenge when using routine programme data is that viral load testing data are only reported for the subset of people who are on antiretroviral treatment. This may underestimate overall population-level suppression, since people not on treatment who naturally suppress the virus will not be included in the numerator. UNAIDS is examining available evidence from cohorts and population surveys to better quantify and adjust for this effect, when reporting on global and regional progress towards the third 95.
UNAIDS, WHO. Guidelines on monitoring the impact of the HIV epidemic using population-based surveys. Geneva: World Health Organization; 2015 (http://www.who.int/hiv/pub/guidelines/si-guidelines-population-survey/en).
Consolidated guidelines on person-centred HIV strategic information: strengthening routine data for impact. Geneva: World Health Organization; 2022 (https://www.who.int/publications/i/item/9789240055315).
Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach Geneva: World Health Organization 2021. https://www.who.int/publications/i/item/9789240031593
Consolidated guidelines on person-centred HIV patient monitoring and case surveillance. Annex 2.4.6: HIVDR EWI sampling, abstraction and reporting guidance. Geneva: World Health Organization; 2017 (https://www.who.int/hiv/pub/guidelines/WHO_Consolidated_Guidelines_Annex...).
Pillay T, Cornell M, Fox MP, Euvrard J, Fatti G, Technau KG et al. Recording of HIV viral loads and viral suppression in South African patients receiving antiretroviral treatment: a multicentre cohort study. Antivir Ther. 2020;25(5): 257–266 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7982353/