(HTS_Index) Number of individuals who were identified and tested using Index testing services and received their results
Export Indicator
This is the first MER indicator to monitor PEPFAR programming of HIV Index Testing services (often also referred to as Partner Notification Services or contact tracing, etc.).
Index testing, also referred to as partner testing/partner notification services, is an approach whereby the exposed contacts (i.e., sexual partners, biological children and anyone with whom a needle was shared) of an HIV-positive person (i.e., index client), are elicited and offered HIV testing services. In this context, index testing refers to any HIV testing of the contacts of an index client (i.e., a person known to be HIV positive). Only the following persons count as contacts: current or past sexual partner(s), biological children /parents (if index case is a child) or anyone with whom a needle was shared. Biological children reported under HTS_INDEX should only include children of an HIV- positive mother. Children of male-index clients (fathers) should only be included when the biological mother is HIV-positive, she is deceased, or her HIV status is not known or not documented. Conversely, if the index client is the child, his/her mother should be tested, and if the mother is HIV-positive or deceased, the father should be tested as well. In addition, all biologic siblings of the index child should be tested. In this way, provision of index testing services is non-directional, whereby we are trying to follow transmission of the disease. Every newly diagnosed individual becomes a subsequent index client from whom to elicit contacts. Like HTS_TST and HTS_SELF, HTS_INDEX is reported at the facility and community levels.
Testing of persons who have not had exposure through an index client, such as neighbors or family members (e.g., children of HIV-negative mother, grandparents, etc.) not born to the index, should not be reported under HTS_INDEX. Testing of non-contacts should be reported under the modality that best reflects the service delivery point where testing occurred. For example, if HIV testing were conducted in a mobile clinic, unexposed contacts would be reported under the ‘Mobile’ modality of HTS_TST.
All index testing services must meet WHO’s 5C minimum standards, including consent, counseling, confidentiality, correct test results, and connection to HIV prevention (for both HIV-positive and HIV-negative individuals), and HIV care and treatment (often referred to as ‘linkage’, for HIV-positive individuals). The 5 C’s are essential for all HTS, especially in the context of identifying contacts for HIV testing. Additionally, all index clients should be screened for Intimate Partner Violence (IPV) per WHO guidelines. An index client should not feel as if they are required to provide contacts in order to receive any services.
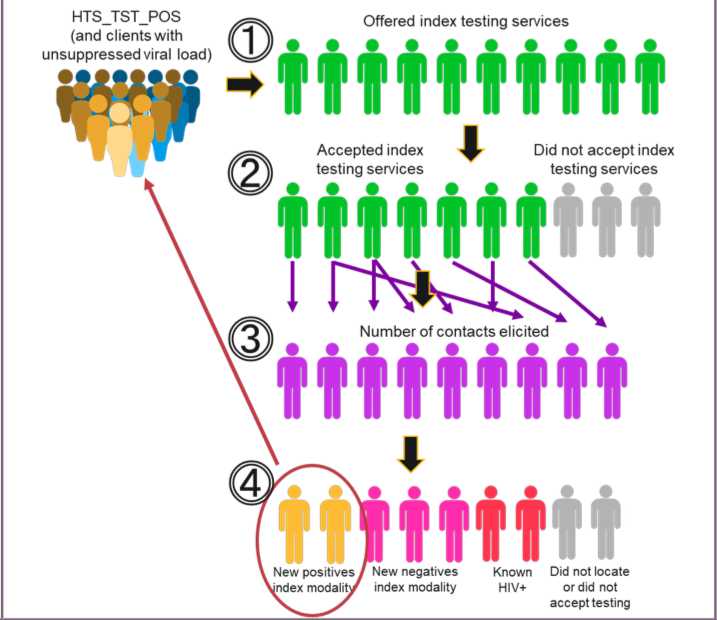
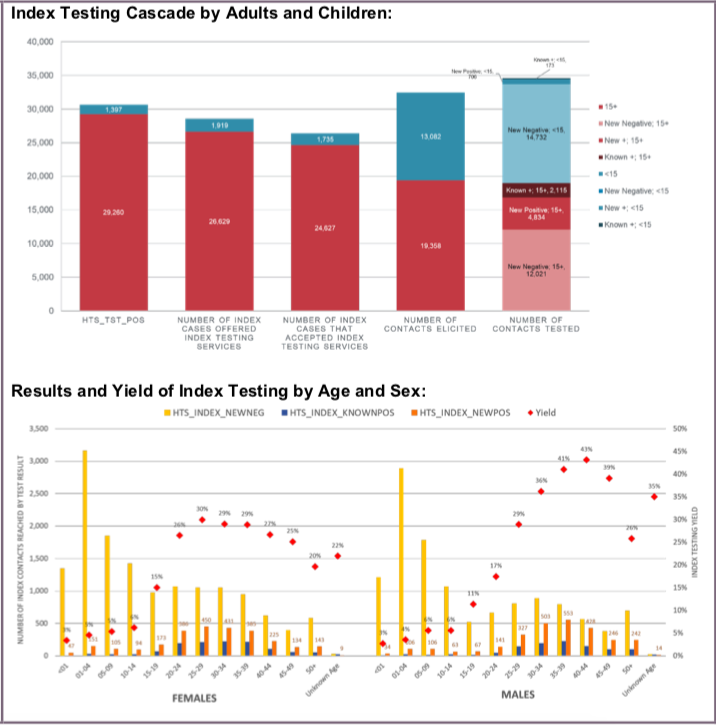
HTS_INDEX is separated into several steps (1-4 below) that are aligned with core components of index testing implementation. These steps are part of a cascade of implementation that begins with an offer of index testing services to the index client and ends in provision of an HIV test (and results) to the contacts named by the index client. This final step 4 (and the age sex disaggregates) will auto-populate into the ‘Index’ modality in HTS_TST for either facility or community.
The steps are:
- How many index clients were offered index testing services? This is the number of index clients (newly diagnosed positive, previously known positives who may or may not be on ART, or clients with unsuppressed viral load) who were offered (e.g., counseled on) index testing services (regardless of whether or not those services were accepted by the index client).
- How many index clients accepted index testing services? This is the number of index clients who accepted (e.g., agreed to) provision of index testing services by a provider (including, counseling on index testing, elicitation of current or past sexual partners/partner notification, etc.).
- How many contacts did the index client provide? This is the number of contacts provided by the index client as a result of accepting index testing services. The index client provides the age (<15 or >15) and sex (male or female) of the contact(s). Since the index client ‘self-reports’ these data, the contact’s recorded age and/or sex does not need to be corrected in Step 3 if differing age/sex information is collected in Step 4. As mentioned above, contacts are only sexual partners, biological children/parents, and anyone with whom a needle was shared.
- How many contacts were tested for HIV and received their results? Of those tested and received their results, how many tested positive and negative? This is the number of contacts who were tested for HIV and received their results (positive and negative). The positive and negative disaggregations do not include the contact’s self-reported status; only the actual provision of an HIV test to the contact. However, please note that previous or known positives are also recorded as “known positive” in Step 4. Known positives should not be retested.
Reporting and use of this indicator should not preclude any other data collection or indicators that may be used to monitor implementation, effects, and outcomes related to HIV index testing services. That is, other data may need to be collected and used by the program to ensure efficient and effective implementation of index testing services either at the facility or community level. For example, to have a more accurate denominator for contacts tested, programs may also collect information about the number of contacts reached among the contacts elicited. Furthermore, of those contacts reached, how many agreed to test for HIV? Programs may also wish to disaggregate the numbers of contacts reached and tested by the four different approaches to index testing (e.g., client, dual, contract, and provider) to see which approaches are most effective. Programs could also track the number of newly diagnosed partners and children linked to HIV treatment.
Number of individuals who were identified and tested using Index testing services and received their results
N/A
How to calculate annual total:
Sum results across quarters.
How to collect:
The suggested data source is a designated HIV Index Testing Services register or logbook. This will allow easier collection of the data for each step in the index testing cascade shown above (see Steps 1-4 above). Alternatively, existing HTS registers, log books, and reporting forms already in use to capture HTS can be revised to include the steps mentioned above and the updated disaggregation categories. Examples of data collection forms include client intake forms, activity report forms, or health registers such as HTS registers, health information systems, and non-governmental organization records.
Other important considerations for reporting on high-fidelity index testing services:
- For a contact to be counted under Step 4, he/she must be tested for HIV and receive their result or be a known positive. That contact could either self-report a known exposure to someone with HIV as their reason for testing, have an index testing referral letter/card/coupon given to them from their HIV-positive partner/family member (client-referral approach), or have been identified during the elicitation process and contacted by a provider. For example, if someone comes to a facility or mobile unit and requests an HIV test and reports a known exposure to someone with HIV as their reason for testing, that person should be counted under HTS_INDEX. Further, that individual’s HIV diagnosis must be confirmed using a nationally validated testing algorithm. For example, an HIV-positive rapid HIV test performed at the community- or facility- level must be confirmed with a second and third (in some contexts) test, which may be performed at the same site or at a different facility. If the confirmatory test is performed at a different facility, then this may require follow-up by implementing partners to confirm the diagnosis before reporting on the Step 4.
- For children <1, only if serologic tests used for diagnostic purposes should they be reported under HTS_INDEX. Serologic tests for screening infants should be excluded (including tests to look for HIV exposure at age 9 months or another time point). For example, you may use the HTS_INDEX <1 disaggregate to report negative diagnostic results if a serologic-based test is used to confirm the absence of HIV infection in infants <1-year-old who have not breastfed for at least 3 months prior to testing. However, since diagnosis of HIV infection in infants is typically based on virologic, and not serologic tests, the general expectation is not to see results in the “<1” disaggregate of the HTS_INDEX indicator. HIV virologic testing of HIV-exposed infants should be counted under PMTCT_EID.
- Programs that utilize the ‘dual-referral’ approach (i.e., the provider/counselor sits with an index client and their partner(s) to assist with disclosure and/or partner testing) may want to offer re-testing to the index client to protect his or her safety. In this case, the index client’s test result should NOT be counted again under HTS_INDEX or HTS_TST. Individuals who undergo couples testing (i.e., neither partner knows their status) should be counted under HTS_TST and the appropriate service delivery modality should be indicated (e.g., ANC).
- The partner elicitation process of index testing is a continuous process. Providers/counselors should follow local SOPs to determine when PLHIV are asked again about any new partners or previous partners that may not have been disclosed by the index client previously.
- Retesting for verification of HIV positive status before or at antiretroviral (ART) initiation should not be counted under HTS_INDEX. Retesting for verification is primarily conducted as a quality assurance activity to avoid misdiagnosis and to ensure those initiated on ART are indeed HIV positive. Therefore, retesting for verification should only be conducted for persons who have received an HIV diagnosis, but have not yet been initiated on ART.
Please refer to HTS_TST for information on Data Quality and reporting considerations that would also apply here.
Key Populations:
Provision of data (on any of the steps outlined above) specific to key populations (FSW, MSM, Transgender people, PWID, and people in prisons and other closed settings) who were tested and received their results should be included but not disaggregated into a separate ‘KP’ disaggregate. That is, there is no separate Key Population disaggregate requested (unlike HTS_TST). The first priority of data collection and reporting of testing for the index client and their contacts, particularly key populations, must be to do no harm. These data must be managed confidentially to ensure the identities of individuals are protected and to prevent further stigma and discrimination of key populations. Please refer to the KP_PREV and PP_PREV indicator reference sheets for more information on working with KPs.
How to review for data quality:
Data should be reviewed regularly for the purposes of program management, to monitor progress towards achieving targets, and to identify implementation and data quality issues.
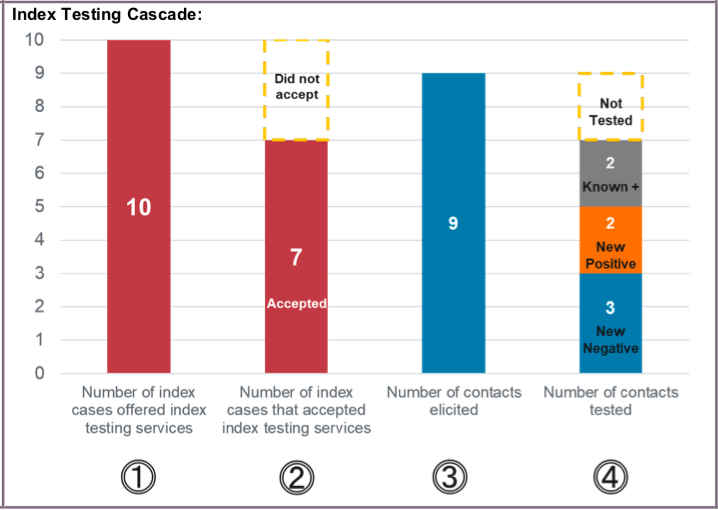
In addition, data reported under each step can be compared to the previous step where it makes programmatic sense. Potential scenarios include: (1) Generally speaking, the number of contacts who were tested for HIV (Step 4) should not be greater than the number of contacts provided (Step 3). Note: testing of a contact of an index client, who was not part of a formal index testing elicitation strategy, may be counted under Step 4 if that contact discloses that his/her sexual or needle-sharing partner is a known positive. (2) Additionally, it is possible for the number of contacts provided by the index client (Step 3) to be greater than the number of index clients who accepted index testing services (Step 2). However, if the number of contacts provided (step 3) is lower than the number of index clients accepting services (step 2), then most index clients are naming zero contacts, which may suggest an issue with the elicitation process.
Reporting level: Facility and Community
Reporting frequency: Quarterly
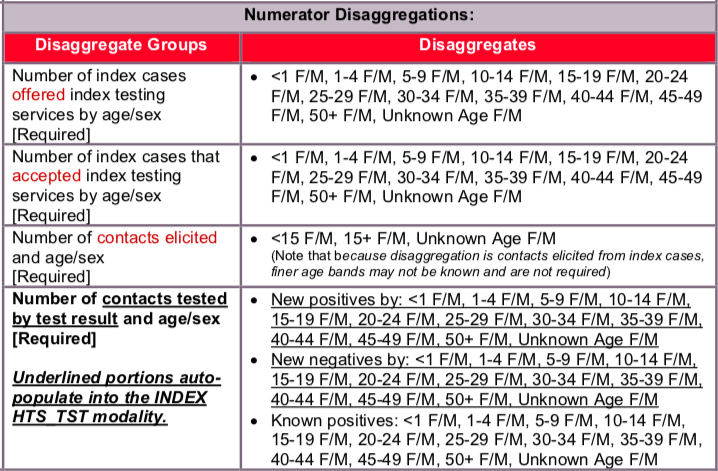
Disaggregate descriptions & definitions:
Please refer to the stepwise process outlined in the “how to use” and “how to collect” sections for more details.
This indicator aims to monitor the scale and fidelity of implementation of HIV index testing-related services
There is no official denominator. However, this indicator represents a cascade and the collected disaggregations serve as both numerators and denominators when analyzing the index testing cascade.
Indicator changes (MER 2.0 v2.3 to v2.4): None
PEPFAR-support definition:
Standard definitions of DSD and TA-SDI apply.
For HTS services, direct service delivery includes: ongoing procurement of critical HTS related commodities such as rapid HIV test kits or requisite materials (lancets, capillary tubes), samples and materials for proficiency testing, other HIV diagnostic commodities, or funding for salaries of HIV testing service providers including counselors, laboratory technicians, program managers, and/or community health workers. Staff who are responsible for the completeness and quality of routine patient records (paper or electronic) can be counted here; however, staff who exclusively fulfill MOH and donor reporting requirements cannot be counted.
For HTS services, ongoing support for service delivery improvement includes: clinical mentoring/supportive supervision, HTS training, HTS guidance development, routine support of HTS M&E and reporting, or HIV test kits consumption forecasting and supply management.
Guiding narrative questions:
- For Step 1, how many previously known positives (versus newly identified positives) were offered index testing services?
- For Step 3, how many contacts were not contacted due to Intimate Partner Violence (IPV) risk? How many contacts were successfully reached, and how? Of contacts reached, how many reported already knowing they were HIV-positive?
- Discuss the contribution of index testing to overall HIV testing conducted within the OU. What are the challenges or facilitators to scaling index testing services over other modalities reported under HTS_TST? Please describe approaches for testing contacts (such as, client-referral, provider referral, contract referral, and/or dual referral) and/or quantify any estimation of linkage to treatment from diagnosis.
Data Visualization & Use Examples:
Related Indicators
TL.4 HTS index testing and partner notification, 2020, WHO Consolidated HIV strategic information guidelines: driving impact through programme monitoring and management (https://www.who.int/publications/i/item/consolidated-hiv-strategic-information-guidelines).