(CXCA_TX) Percentage of cervical cancer screen-positive women who are HIV-positive and on ART eligible for cryotherapy, thermocoagulation or LEEP who received cryotherapy, thermocoagulation or LEEP
Export Indicator
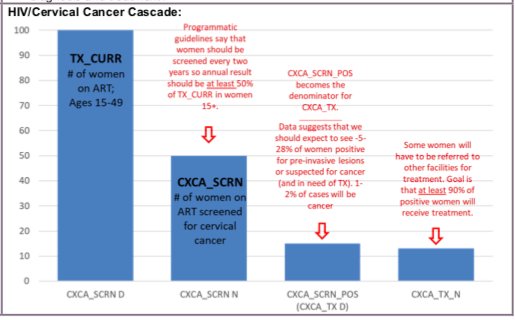
It is vital that all HIV-positive women on ART requiring treatment for precancerous lesions receive the treatment for which they are eligible. The purpose of this indicator is to monitor whether women requiring (and eligible for) treatment for precancerous lesions received treatment.
The globally accepted benchmark of at least 90% eligible for treatment of precancerous lesions receiving treatment should be used when monitoring performance (WHO, 2013; ACCP, 2004).
Number of cervical cancer screen-positive women who are HIV-positive and on ART eligible for cryotherapy, thermocoagulation or LEEP who received cryotherapy, thermocoagulation or LEEP
Number of HIV-positive women on ART at PEPFAR supported sites who are eligible for cryotherapy, thermocoagulation or LEEP, in other words CXCA_SCRN_POS
How to calculate annual total: Sum results across both reporting periods for the numerator
How to collect:
The primary data sources for this indicator are registers or logbooks in use at the point of precancerous lesion treatment service delivery. Client and facility level data collection tools should include the data elements required for disaggregation.
Data for the numerator should be generated by counting the total number of HIV-positive women on ART who received precancerous lesion treatment (cryotherapy, thermocoagulation or LEEP or other) who were eligible for that treatment.
Challenges may arise in counting when women are referred for LEEP, but who are found eligible for cryotherapy (or thermocoagulation) upon presenting at the LEEP service delivery point. It is vital that facility level data collection and program monitoring tools capture the data elements necessary to identify this key performance issue, which can lead to data quality issues for this indicator.
How to review for data quality:
The numerator for this indicator should not be larger than CXCA_SCRN and should be equal to 100% or less of the CXCA_SCRN_POS disaggregate (not including suspected cancer).
Reporting level: Facility
Reporting frequency: Semi-Annually
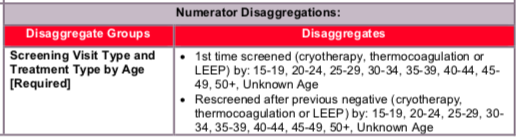
Disaggregate descriptions & definitions:
Treatment type:
- Cryotherapy
- The primary outpatient ablative treatment for small precancerous cervical lesions
- By applying a highly cooled metal disc (cryoprobe) to the cervix and freezing the abnormal areas (along with normal areas) covered by it, cryotherapy eliminates precancerous areas on the cervix by freezing
- Thermocoagulation
- An outpatient ablative treatment for small precancerous cervical lesions that is used instead of cryotherapy in some settings.
- It uses electricity to generate temperatures of 100–120 °C for ablation of cervical lesions and can be used for all stages of cervical cancer.
- LEEP
- The primary outpatient treatment for large precancerous cervical lesions
- The removal of abnormal areas from the cervix and the entire transformation zone,
using a loop made of thin wire powered by an electrosurgical unit; the loop tool cuts and coagulates at the same time; this is followed by use of a ball electrode to complete the coagulation
Screening Visit Type:
- 1st Time screening
- This disaggregate allows the monitoring of screening service provision (and positivity rate) in the screening-naïve HIV-positive population – only women being screened for the first time in their lifetime should be counted under this disaggregate.
- Rescreening after previous negative result
- This disaggregate allows the monitoring of screening service provision (and positivity rate) in the population of HIV-positive women who have received at least one cervical cancer screening test in their lifetime, and who received a negative result on their most recent screening test
- WHO recommends that HIV-positive women or women of unknown HIV status who receive a negative cervical cancer screening test result be rescreened every 3 years; however, the results of PEPFAR modelling exercises led to the current PEPFAR recommendation of a screening interval (for women with a negative result) of every 2 years for HIV-positive women
- As a program matures, countries should consider adding an additional performance indicator which measures whether women that should return for routine rescreening in a given time period are returning in that time period (e.g., number of rescreened women in a given time period, over the number of women who were expected to be rescreened in the same time period)
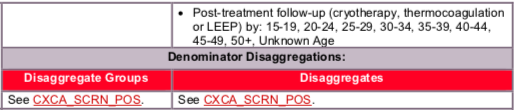
- Post-treatment follow-up screening
- This disaggregate allows the monitoring of screening service provision (and positivity rate) in the population of HIV-positive women who have received at least one cervical cancer screening test in their lifetime, and who received precancerous lesion treatment due to a positive screening result on their last screening test
- Some national guidelines require post-treatment follow-up screening at intervals other than or in addition to 1 year (e.g., 6 months and 12 months) – programs should use additional indicators to monitor the additional follow-up time points, and this should be noted in the narrative
The numerator captures the number of individual HIV-positive women on ART who required treatment for precancerous cervical lesions, who received that treatment.
See CXCA_SCRN_POS
Indicator changes (MER 2.0 v2.3 to v2.4): None
PEPFAR-support definition:
Standard definition of DSD and TA-SDI used.
For precancerous cervical lesion treatment services, direct service delivery includes: ongoing procurement of critical treatment related commodities such as carbon dioxide or nitrous oxide gas or requisite materials (cryotips, specula, spatulas and swabs, exam gloves, etc.), or funding for salaries of precancerous lesion treatment service providers including program managers, supervisors, and/or coordinators. Staff who are responsible for the completeness and quality of routine patient records (paper or electronic) can be counted here; however, staff who exclusively fulfill MOH and donor reporting requirements cannot be counted.
For precancerous cervical lesion treatment services, ongoing support for service delivery improvement includes: clinical mentoring/supportive supervision, cryotherapy, thermocoagulation or LEEP training, guidance development, infrastructure/renovation of facilities, site level QI/QA, routine support of M&E and reporting, or commodities consumption forecasting and supply management.
Guiding narrative questions:
- Please describe challenges with the provision of same day treatment and/or with the return of women who postpone precancerous lesion treatment.
- At sites where both thermocoagulation and cryotherapy are offered, what if any context is given by women choosing one treatment option over the other?
- Please provide a summary of the outcomes of all women with suspected invasive cervical cancer. How many were seen at the referral site, how many were found to have invasive cancer? Of those with invasive cancer, how were they treated? Have there been any deaths from cervical cancer among women on ART? What are the barriers to diagnosis and treatment?
Data Visualization & Use Examples: