HIV expenditure by origin of resources
Export Indicator
In-country expenditures of HIV programmes and services by source in a standardized and comparable manner according to mutually exclusive categories. The HIV expenditures by programme or service reported here would need to be consistent with the number of people who have received the services (as reported elsewhere in Global AIDS Monitoring).
The indicator to be reported is total and subtotal HIV expenditures by services or programme categories and by financing sources. There are eight core sub-indicators that map to this reporting. These are outlined under Annex 3.
By the end of 2020, the international and domestic resource availability for the HIV response reached an estimated US$ 21.5 billion (in constant 2019 dollars) in low- and middle-income countries. Achieving country and global targets requires increased focus, resources, programme effectiveness and efficiency to provide the HIV care, treatment and prevention to reduce HIV incidence and extend life.
It is critical to identify long-term, sustainable financing sources, including domestic resource mobilization, to maintain and build upon the success achieved. However, filling the financing gap and pursuing efficient resource allocation can only be achieved by assessing and managing the resources available and their use.
The quantification of financing flows and expenditures helps to examine the questions of who benefits from HIV programmes and to determine the current state of allocations for HIV programmes and services that focus on key or other specific populations.
The vast majority of the AIDS Spending Categories (or ASCs, per National AIDS Spending Assessment [NASA] classifications) or the sub-indicators are drawn from existing frameworks and are now structured around the 2021 Political Declaration on Ending AIDS. The resource needs for low- and middle-income countries resulted in a target to mobilize at least US$ 29 billion (in constant 2019 US dollars) by 2025.
Not applicable
Not applicable
Data type
Currency and monetary values (nominal currency)
Social accounting and costing principles need to be applied for producing expenditure data. Rules, frameworks and principles are described in the specific manuals and guidelines (links provided below).
The calculation of each service/programme or sub-indicator may have individual characteristics to ensure proper accounting of all components (e.g., direct and shared costs of service provision) and to avoid double-counting; these calculations may be different by each financing source and service delivery modality (or even by service provider). Further guidance is available in the respective guidelines and manuals listed at the end of this section.
The quantification is limited to in-country expenditures, using international development assistance funds and the expenditures incurred using public or private funds reported in the current US$ or local currency units for the chosen reporting year.
There are certain requirements for data collection and quality to ensure the reliability and validity of the indicators to assure credibility.
The conciliation of top-down estimates (from the financing sources) and bottom-up (from the costing of service delivery) provides the best assessment of the total HIV in-country spending.
Financial and programme records from providers or service delivery organizations are the basis for data collection.
There are significant documented discrepancies between budgetary allocations and actual expenditures. Budget analysis is not recommended as the sole basis for reporting total in-country HIV expenditure.
It is good practice to validate expenditures funded by international sources, national financing sources and financing agents, as well as with all relevant stakeholders.
- National AIDS Spending Assessment (NASA).
- Budget analysis.
- System of Health Accounts 2011 (SHA-2011) with HIV module.
- When a NASA is not available, countries may use centrally produced results from the PEPFAR expenditure reporting system and request expenditure data from the Global Fund, that can be made available to reporting countries as a part of global coordination and resource alignment across UNAIDS, PEPFAR and the Global Fund. The reporting of expenditures for programmes funded by the Global Fund must conform to the reporting guidelines on Progress Update and Disbursement Request. (Please see Progress Update and Disbursement Request Form Instructions (https://www.theglobalfund.org/media/11754/fundingmodel_pudr_instructions...))
- Health accounts using the SHA-2011 framework with full disease distribution attempt to capture top-level aggregated programme categories with cost item. However, depending on the objectives of a given resource-tracking exercise, SHA-2011 may or may not inform on the totality of HIV granular expenditure (disaggregated by programme) as required, and applied distribution keys must be examined and updated if necessary. The countries’ health account report and data may have to be supplemented by robust costing principles to disaggregate the HIV portion of the joint costs incurred by the system.
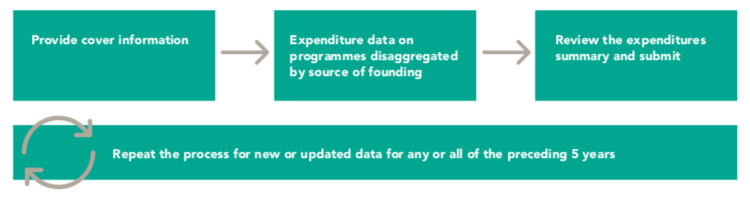
The amended data for previous years can be submitted if the data submitted in previous years were preliminary or were not submitted previously.
Annually for calendar or fiscal year. Since the results of any accounting exercise may take time longer than the deadline for annual reporting, countries may submit preliminary results, which will be substituted when final results are available. In this reporting cycle, we suggest that countries submit any number of annual final reports available from the last five years, indicating their status as preliminary or final and whether they substitute for previous reports. It is not required to resubmit the data that have previously been reported and that remained unchanged. The UNAIDS team can be contacted for assistance if countries would like to submit recently amended or final reports on expenditures prior to 2016.
- Financing source.
- HIV and AIDS programme categories.
- For selected sub-indicators, countries are encouraged to report expenditures on the most salient commodities under each of the relevant programmes representing sub-indicators, as data allow. Reporting of total expenditures by programme is acceptable if the dissagregation is not known but there is certainty that both commodities and service delivery costs are included.
Countries that have appropriately implemented a full NASA are able to fill the template with an output table from the NASA exercise. Final country estimates need to be validated with all stakeholders and triangulated to increase reliability and validity.
Countries that have implemented an SHA-2011 annual exercise may need to ensure that the allocation keys used to estimate HIV expenditures from the utilization of the health system are updated and allow the granular data for domestic sources. This process may not use certified data as some accounting principles might require. Countries that have just started the process of full distributional health accounts need to validate the results with other existing sources and all stakeholders to increase reliability and validity of the estimates, particularly the overall level, potential duplication and significant unaccounted expenditures. Countries using health accounts should add non-health-related expenditures and ensure that consistent HIV expenditure is reported, particularly for shared costs in the health system. The implementation of health accounts needs medium- to long-term planning, and it is resource-intensive and depends on coordination between health accountants and programme managers.
Countries using budget analysis need to ensure that allocated budgets were spent as planned; the estimates for the expenditures that are not incurred using an earmarked budget should be added to each subtotal, as appropriate.
Countries have the choice of reporting on: (a) separate costs (commodities and service delivery) if they have the data; (b) on only one cost (if that is what is available); or (c) a dissagregated total that includes both commodities and service delivery.
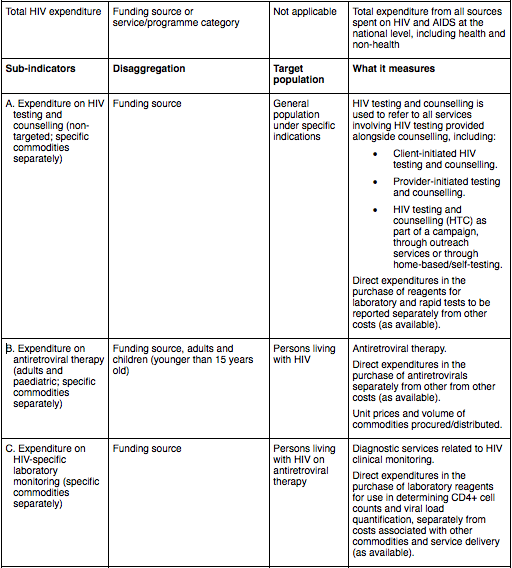
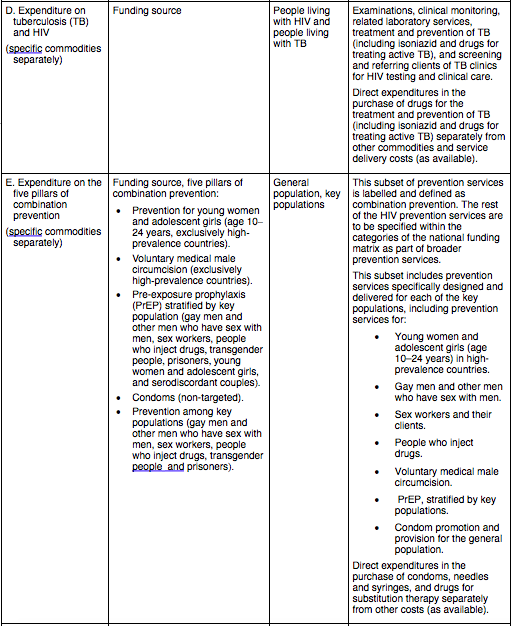
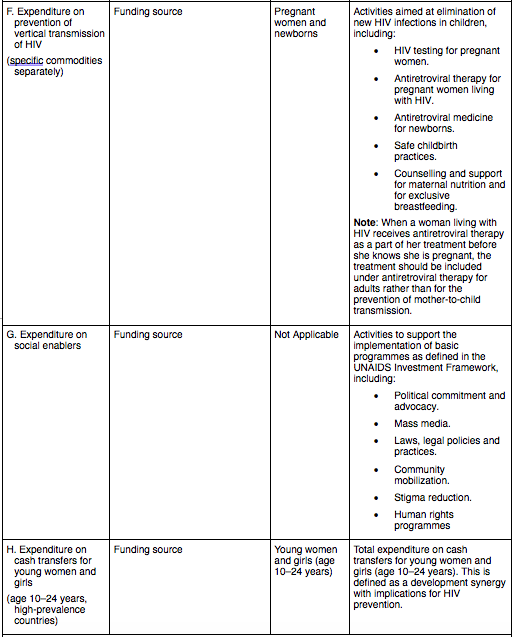
List of core sub-indicators and associated statistical metadata
To access guidelines, framework tools and classifications for NASAs, please contact AIDSspending@unaids.org
Health Accounts reports are available at the World Health Organization (WHO) Global Health Expenditure Database: http://apps.who.int/nha/ database/DocumentationCentre/Index/en
Eurostat. HEDIC – Health expenditures by diseases and conditions. 2016 edition [Internet]. Luxembourg: Publications Office of the European Union; 2016 (http://ec.europa.eu/eurostat/web/products-statistical-working-papers/-/K...).
For more information on this indicator, please see the Annexes of the Global AIDS Monitoring (GAM) guidelines.
For more information on the background and guidance to reporting, with emphasis on in-country collaboration and process, please see the Global AIDS Monitoring Framework 2022-2026.