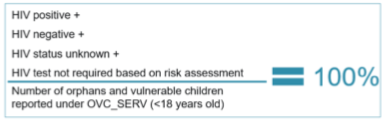
(OVC_HIVSTAT) Percentage of orphans and vulnerable children (<18 years old) with HIV status reported to implementing partner
Export Indicator
This indicator will be tracked through routine program monitoring semi- annually through the POART process.
Given the elevated risk of HIV infection among children affected by and vulnerable to HIV, it is imperative for PEPFAR implementing partners to monitor HIV status among OVC beneficiaries, to assess their risk of HIV infection, and to facilitate access and retention in ART treatment for those who are HIV positive. When the implementing partner determines that the child is at risk of HIV infection, the program should refer children for testing and counseling services. When the implementing partner knows the HIV status, the program should ensure that the children are linked to appropriate care and treatment services as an essential element of quality case management. OVC programs should also play an important role in family-centered disclosure, for those who are HIV positive. The goal of monitoring OVC_HIVSTAT is to increase the proportion of children reported as active or graduated under OVC_SERV under age 18 with a known HIV status or for whom an HIV test is not required based on a risk assessment.
- This indicator is NOT intended to be an indicator of HIV tests performed or receipt of testing results, as these are measured elsewhere, and confirmed test results are frequently unavailable to community organizations due to health facility concerns about patient confidentiality.
- This indicator is NOT intended to imply that all OVC beneficiaries require an HIV test. OVC with known positive or negative status do not need to be tested. OVC with unknown HIV status should be assessed for risk, and if determined to be at risk, should be referred or otherwise supported, to access HTS. For younger children who are determined not to be at risk (“test not required based on risk assessment”) reassessment of risk will only be needed in cases where their risk situation changes (i.e., in cases of child sexual abuse). Older children whom the IP thinks may be sexually active should be assessed every reporting period. An HIV risk assessment should always occur prior to HIV testing to determine if a test is required.
- Status disclosure to the implementing partner is NOT a prerequisite for enrollment or continuation in an OVC program. OVC programs serve persons of positive, negative, and unknown HIV status appropriate to their needs and vulnerability to HIV. This indicator ensures that IPs are regularly providing outreach to caregivers to identify children’s HIV status, encouraging family disclosure, and linking to care and treatment services as needed.
- This indicator captures if implementing partners are tracking the self-reported HIV status of the OVC that they serve and enrollment in ART for those who are positive. Testing results for OVC who are referred for testing should be reported under HTS_TST based on the service delivery point where they are tested.
- This indicator also captures if implementing partners are tracking if the OVC that they serve who report to be HIV positive are successfully linked to and retained in treatment and care. ART treatment status should be recorded both at the time of enrollment as well as at regular intervals at least once during the reporting period.
- Since this is not a testing indicator, HIV positivity yield should NOT be calculated based on this indicator. Yield calculations should only be made by testing partners.
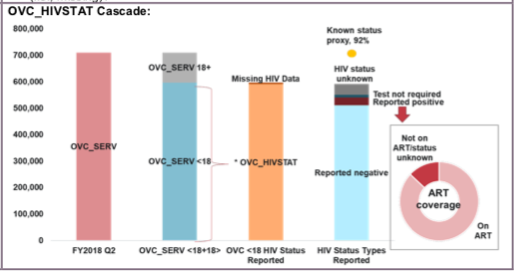
- A helpful way to assess OVC_HIVSTAT performance is to create a “known status proxy” category of known status/risk (by combining those reported positive, negative, and those who have been risk assessed and found to not require a test) and compare this with OVC_SERV <18. This analysis encourages programs to actively follow-up on all instances of “HIV status unknown” by targeting instances of missing data, nondisclosure, and issues with reporting timing. While OVC_HIVSTAT as a percentage of OVC_SERV <18 historically intended to identify gaps in IP tracking of HIV status of OVC, this updated way of reviewing the data provides insight into OVC with known status and identifies where additional follow-up is needed for those with unknown status.
- This indicator is a subset from OVC_SERV. Only OVC who were reported under OVC_SERV <18 should be included in the denominator for this indicator.
- DREAMS beneficiaries under 18 who are reported under OVC_SERV should also be reported under OVC_HIVSTAT where feasible, as should beneficiaries of 9-14 primary prevention of sexual violence and HIV interventions.
Number of orphans and vulnerable children (<18 years old) with HIV status reported, disaggregated by HIV status
Number of orphans and vulnerable children reported under OVC_SERV (<18 years old, total numerator including active and graduated)
How to calculate annual total:
This is a snapshot indicator. Results are cumulative at each reporting period.
Implementation of the HIV risk assessment should be integrated into case management and on-going case monitoring, and should not be conducted separately, if possible. This will vary by partner and project. The partners should work out a timeline based on their experience of how long referral completion and status disclosure usually takes and factor that into their case management processes.
Implementing partners will record the OVC beneficiary’s self-reported HIV status semi- annually.
Reporting Scenarios:
Q1. Daniel reports to the community health worker (CHW) that he is negative, but his last test was two years ago. Is Daniel still reported as “Negative”, or as “No Status”, and needs to be risk assessed?
A1. Based on their knowledge of the child from case management records, if the CHW believes that the child has no risk of HIV infection (i.e., no one in the household is HIV+, they are not exposed to violence, child is not sexually active yet) then getting another test done is not necessary and would report them as negative. This applies mainly to younger children under age 12 (depends on average age of sexual debut in the country). For adolescents, we recommend getting risk assessed if the test was not conducted in the reporting period.
In that same scenario, what if the CHW decides to administer the HIV Risk Assessment to Daniel and finds that an HIV test is not indicated, how should that be reported? This should be reported as “Test Not Required Based on Risk Assessment” because once the CHW decides to conduct a risk assessment, this means that the child’s status is in question and that should be captured as No Status.
Q2. Elizabeth reports to the CHW that she is negative and had an HIV test within the past 6 months, but the CHW knows that she was recently exposed to something that could put her at high risk (e.g., GBV, sexually active), what should the CHW do?
A2. Because the CHW thinks that Elizabeth may be at risk of HIV infection, the CHW would conduct the risk assessment and she is no longer reported as “Reported HIV Negative”. If found at risk (e.g., GBV exposure) then she should be referred for testing. If determined to be Test Not Required Based on Risk Assessment Elizabeth would be captured as “Test Not Required Based on Risk Assessment”.
If she completes the testing within the reporting period and the caregiver is willing to disclose the result of the test, her response would be captured accordingly.
If she is risk assessed and referred for testing, but her caregiver is not able/willing to complete the test or disclose the status within the reporting period it is captured as “No HIV Status”. Hopefully by the following reporting period, the caregiver will have completed the referral and disclosed the child's status so it can be captured as positive or negative. It is understandable that the whole process from risk assessment to referral completion and disclosure may not be completed within 6 months and there be movement from “No HIV Status” to “Reported HIV positive” or “Reported HIV Negative” in future reporting periods.
Q3. What do we do when a caregiver refuses to disclose their status and the status of their child or refuses to complete an HIV test – even when the HIV risk screening tool indicates that their child is at high risk of HIV infection?
A3. A caregiver should never be forced to disclose their or their child’s status, the results of an HIV test, or to complete an HIV test. HIV status and completion of an HIV test are not required for enrollment in an OVC program. If a child is believed to be at high risk of HIV and the caregiver is reluctant to disclose results or complete a test, OVC programs should attempt to facilitate a meeting with the caregiver, and persons specially trained on HIV disclosure. OVC programs may also consider enlisting the support of community members with whom the caregiver has greater trust. Until the client chooses to disclose test results, status under OVC_HIVSTAT should be recorded as “No HIV Status.”
Q4. How do we report on HIV exposed infants who are still too young to have had their final HIV status testing?
A4. Because HIV-exposed infants may be tested at multiple points prior to receiving a final HIV status, we recommend that they be counted as "no status" until such time that the clinic determines their final status as positive (infected) or negative (not infected). A note can be entered in DATIM in the narrative section indicating the number of children entered as "no status" that are HIV-exposed (i.e., infants during the reporting period who were of undetermined status). It is important for all HIV-exposed infants and their caregivers to be facilitated to make appointments deemed necessary by the clinic.
The OVC_HIVSTAT total numerator should equal OVC_SERV<18 results total numerator, including active and graduated. Review any site with the following reporting issues: 1) numerator greater than 100% of OVC_SERV <age 18, and 2) very low coverage of OVC_HIVSTAT (defined as OVC_HIVSTAT numerator divided by OVC_SERV <18) which provides data on reporting of status.
Missing data should be documented under “HIV status unknown” or “Reported HIV positive- Not currently receiving ART or ART status unknown.” Potential reasons for missing data may include: 1) IP was not able to collect information from all caregivers of OVC_SERV<18 within the reporting period, 2) IP was not able to locate all the caregivers of OVC_SERV<18 (e.g., relocated, migrant work).
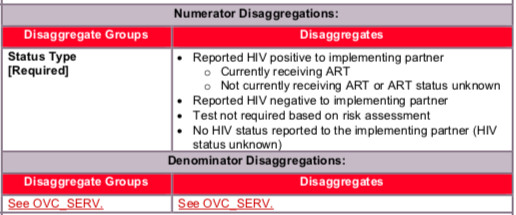
Disaggregate descriptions & definitions:
Status Type Disaggregate Definitions:
- “Reported HIV positive to IP” includes beneficiaries <age 18 who report to the IP that they are HIV positive based on an HIV test conducted during or prior to the reporting period (regardless of where the test occurred). All beneficiaries <age 18 who report to the IP that they are HIV positive based on an HIV test conducted during or prior to the reporting period (regardless of where the test occurred) should be reported as “currently receiving ART” or “not currently receiving ART or ART Status Unknown”. This also includes beneficiaries <age 18 who report that they are HIV positive based on an HIV test conducted during previous project reporting periods. OVC entered in either category as “Reported HIV positive– currently receiving ART” or “Reported HIV positive– not currently receiving ART or ART Status Unknown” in the previous reporting period should be followed in the current reporting period and their current ART treatment status noted. In order to be counted as “currently receiving ART” the IP should confirm at the last visit preceding the reporting month whether the response to the following questions is “yes” to ensure that this captures more than just initial linkage to care: Do you have enough ART pills to take until the date of your next appointment?
- “Reported HIV negative to IP” includes beneficiaries <age 18 who report that they are HIV negative to the IP based on an HIV test conducted during the reporting period (regardless of where the test occurred). For a child who reports multiple tests within the current period, use most recent test. For beneficiaries entered as “Reported HIV negative to IP” in a previous reporting period—if the IP believes the child’s risk has not changed in the last six months, they should continue to report the child as negative during the current reporting period. However, if the IP believes that the child has recently been exposed to risk of HIV infection (e.g., sexual violence) or if an adolescent has become sexually active, then the IP should conduct the HIV risk assessment. Potential outcomes reported after the HIV risk assessment include 1) the child is tested and reported as HIV positive and either currently receiving ART or not receiving ART or ART status unknown, or 2) the child is tested and reported as HIV negative, 3) the child is reported as “No HIV Status reported to the IP”, or 4) the child is reported as “Test not required based on risk assessment.”
- “Test not required based on risk assessment” includes beneficiaries (OVC_SERV<age 18) who based on a risk assessment made by the implementing partner do not require a test during the reporting period (formerly known as test not indicated). (Consensus Conference Technical Report on the Role of OVC Programs Supported by PEPFAR in Extending Access to HTS includes further information on determining whether a test is required).
- “No HIV status reported to the IP” (HIV status unknown) includes all beneficiaries <age 18 who do not fit in the above categories and who report to the IP that they do not know their HIV status or for whom HIV status is missing. Potential scenarios for reporting a child in this category include:
- Not yet assessed: Child enrolled in program, but not yet assessed for HIV risk.
- Refuse HIV assessment: Caregiver has been approached, but did not agree to let the IP conduct a risk assessment on the child in the reporting period.
- At risk for HIV: Child has been assessed and is at risk for HIV, but caregiver has not yet taken child to be tested (including if they have refused testing referral or if they have accepted the referral but not yet completed the test).
- HIV referral completed: OVC has completed HIV test, but result is not available OR caregiver doesn’t report results to IP in the reporting period.
- Refuse report: Caregiver has been approached by IP but have not yet agreed to disclose whether the child has been tested and his/her current HIV status in the reporting period
- Missing: No available data, including because an IP did not attempt to find out about a child’s status.
We recommend that IPs aim to move a newly enrolled OVC with HIV Status Unknown through the assessment cascade within the reporting period. A newly enrolled child would initially be considered “HIV Status Unknown” until he/she is risk assessed. If the OVC is found to not be at risk at present, he/she will be noted as “Test not required based on risk assessment.” If the OVC is found to be at risk, he/she will be referred for HIV testing and then the program will work with the guardian to disclose the results until he/she can be reported as “Reported HIV Negative”, “Reported HIV Positive – currently on ART” or “Reported HIV Positive – not currently on ART or ART status unknown”.
For children reported as ”HIV Status Unknown” in the previous reporting period, the IP should ensure that child is risk assessed, referred for testing if needed, and supported to disclose new test results. Children reported as “Test not required based on risk assessment” with no changes in their risk situation for the past six months, don’t need to be reassessed. If the IP believes the child’s risk situation has changed in the last six months, then the child should be reassessed by the implementing partner to determine whether testing is indicated and the results entered as outline above, and the child should receive appropriate follow-up.
Data sources for this indicator include HIV test results that are self-reported by OVC (or their caregivers), results of HIV Risk Assessments conducted by implementing partners, registers, referral forms, client records, or other confidential case management and program monitoring tools that track those in treatment and care.
Denominator is not collected again as part of this indicator, but is collected under the indicator OVC_SERV.
Indicator changes (MER 2.0 v2.3 to v2.4):
Minor clarifications have been made to the indicator reference sheet, including further defining “currently receiving ART” under the “Reported HIV Positive – Currently receiving ART” disaggregate.
PEPFAR Support definition:
Modifications to standard definition of DSD and TA-SDI related to eligible goods and services:
Provision of key staff or eligible goods/services for OVC beneficiaries receiving care and support services in the community include: For beneficiaries of OVC services, this can include funding of salaries (partial or full) for staff of the organization delivering the individual, small group or community level activity (e.g., psychosocial support, child protection services, education, etc.). Partial salary support may include stipends or incentives for volunteers/para-social workers or paying for transportation of those staff to the point of service delivery. For goods or services to be eligible, goods or services (e.g., bursaries, cash transfers, uniforms) can either be paid for out of the implementing partner’s budget or be provided as a result of the IP’s efforts to leverage and mobilize non-project resources. For example, an IP may help beneficiaries fill out and file forms necessary for the receipt of government provided cash transfers, social grants, or bursaries for which they are eligible. Given the focus on long-term local ownership, IP’s are encouraged to mobilize goods and services whenever possible.
For care and support services, ongoing support for OVC service delivery for improvement includes: the development of activity-related curricula, education materials, etc., supportive supervision of volunteers, support for setting quality standards and/or ethical guidelines, and monitoring visits to assess the quality of the activity, including a home visit, a visit to a school to verify a child’s attendance and progress in school or observation of a child’s participation in kids clubs.
Guiding narrative questions:
- If the sum of reported HIV negative + reported HIV positive + Test not required based on risk assessment is less than 90% of OVC_SERV <18, please explain why such a high proportion are being reported in the category of “HIV Status Unknown” (i.e., the performance metric described in the “how to use” section). Are there certain partners that are struggling with reporting or understanding the disaggregates? How is the Mission responding?
- Please explain the breakdown of those reported under “HIV Status Unknown.” What percentage of caregivers refused to disclose a child’s HIV status? What percentage represents those who have been referred for testing but do not yet have results? What percentage represents missing data where an implementing partner failed to document the child’s HIV status? What are other reasons (and corresponding percentages) (e.g., 9-14 year-olds only receiving primary prevention of sexual violence interventions who were not risk assessed)?
- For children reported as “Reported HIV Positive - not currently on ART or ART Status Unknown”, what efforts are being undertaken in response? Are there certain partners with low ART coverage, why? Is this an issue related to community case management? Or are partners having a hard time collecting timely confirmation of treatment status (i.e., missing)?