(KP_PREV) Number of key populations reached with individual and/or small group-level HIV prevention interventions designed for the target population
Export Indicator
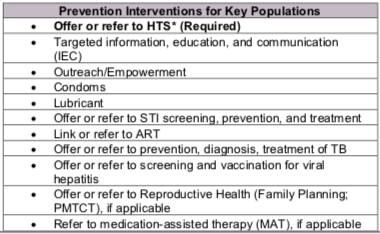
Number of key populations reached with individual and/or small group-level HIV prevention interventions designed for the target population
N/A
How to calculate annual total:
Sum across both reporting periods; de-duplicating unique individuals already reached and reported in Q1-Q2 of the same fiscal year in Q4 reporting.
How to collect:
Tracking systems must be able to reduce double-counting of individuals in a reporting period. The numerator can be generated by counting the number of de-duplicated individuals who were reached and had completed the appropriate prevention intervention(s) designed for the intended key population. For example, this means that when a unique individual receives HTS referral plus condoms and lubricant at more than one occasion during the reporting period, the person is counted only once for being reached for this indicator.
Furthermore, de-duplication of all returning beneficiaries within the Q3-Q4 reporting period (April 1 – September 30) will also need to take place in Q4 reporting if they had already been counted under KP_PREV in Q1-Q2 of the same fiscal year. For example, if an individual had received prevention interventions under KP_PREV through PEPFAR-supported program in January 2017 and was counted as being reached in FY17 Q2 reporting cycle, and this same individual was later reached with prevention services again by PEPFAR-supported program in June 2017, that individual should NOT be reported again in the FY17 Q4 reporting period. This de-duplication is critical to accurately track the ANNUAL number of unique individuals reached by PEPFAR within a given fiscal year. Trend analysis of past performance of KP_PREV data will be adversely affected with the change in frequency of KP_PREV reporting from annually to semi-annually if this de-duplication is ignored (i.e., annual number of KP_PREV reported within the same fiscal year would be inflated as the same individual would be counted twice if this de-duplication does not occur at Q4 reporting).
If possible, a unique identifier can be assigned. The use of a unique identifier can help programs monitor the frequency of contact/outreach of a single individual over time (i.e., Beneficiary A with unique identifier AW0901 had four documented outreach visits in FY17 but was only counted once under KP_PREV in FY17).
How to review for data quality:
- Numerator
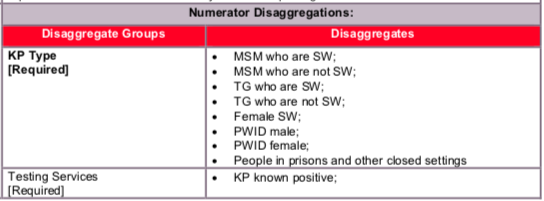
- The Numerator is = to the sum of the disaggregation: The number of KP reached with individual and/or small-group level preventive interventions should be equal to the sum of KP disaggregates.
- Despite persons potentially falling into more than one KP disaggregate (e.g., FSW who injects drugs), implementing partners should be instructed to report an individual in only one KP category with which s/he is most identified.
Reporting level: Facility & Community
Reporting frequency: Semi-Annually
Disaggregate descriptions & definitions:
- Known Positive: Persons within each key population type for whom HIV testing is not indicated because they are known to be HIV-positive. HIV-positive test results should be verified, if possible, for all persons accessing HIV prevention services during the reporting period. Implementing partners should maintain records (without personally identifiable information) on whether the HIV-positive client is linked to treatment. Patients tested positive in previous reporting periods should be counted as Known Positives.
- Newly Tested and/or Referred for Testing: Persons within each key population type for whom HIV testing is indicated because they do not know their HIV status or their last HIV-negative test was more than 3-6 months ago (or more/less frequently as indicated by National Guidelines) should either be offered an HIV test on site or given information about where and when they can access an HIV test at another nearby clinic. Every attempt should be made to ensure the client is linked with HIV testing services that are KP-friendly, and where possible the completed referral should be documented (i.e., the client accessed HIV testing). Note: Persons who access testing and whose results are newly tested HIV-positive in the reporting period should also be counted under “newly tested” even if they return for additional prevention services during that reporting period.
- Declined Testing and/or Referral: Persons who, after explaining the benefits of HIV testing and the reason for testing every 3-6 months (or more/less frequently as indicated by National Guidelines), decline to be tested on-site or referred to a site where HIV testing is offered. Although every attempt should be made to support key populations with HIV testing as part of the package of HIV prevention services and to provide HIV testing on site or KP-friendly sites, programs should also respect the autonomy of clients to decline this service. Clients who decline testing and/or referral can still receive other prevention services, as long as the benefits of HIV testing were explained and testing or a referral for testing was offered.
The numerator can be generated by counting the number of unique individuals from an activity who are reached with prevention interventions designed for the intended key population.
Indicator changes (MER 2.0 v2.3 to v2.4): None
PEPFAR Support definition:
Standard definition of DSD and TA-SDI used.
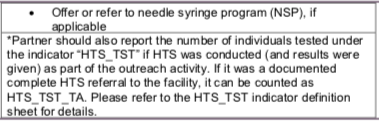
Provision of key staff or commodities for KP receiving HIV prevention services include: ongoing procurement of critical commodities such as test-kits, condoms, lubricants, or funding for salaries of personnel providing any of the prevention package components (i.e., peer navigators, outreach workers, program managers). Staff responsible for the completeness and quality of routine patient records (paper or electronic) can be counted here; however, staff who exclusively fulfill MOH and donor reporting requirements cannot be counted.
Ongoing support for HIV prevention among KP improvement includes: mentoring and supportive supervision; training; organizational strengthening; QA/QI; program design like development of training curricula, prevention guidance development, or standard operating procedures (SOPs) and follow-up to ensure fidelity to the program design; regular assistance with monitoring and evaluation functions and data quality assessments; or condom forecasting and supply management.
Guiding narrative questions:
- Did the IMs de-duplicate all returning beneficiaries in Q3-Q4 who have already been counted in Q1-Q2 of this fiscal year? If not, why not?
- Are there mechanisms in place (i.e., unique identifier) in which IMs can de-duplicate multiple outreach encounters within a fiscal year? What are these mechanisms? If mechanisms are not in place, how does the IM report individuals and not encounters within the fiscal year?
- Do the testing service disaggregations equal the total number of KP_PREV reported? If not, why not?
- What were the barriers in collecting testing service disaggregations for this indicator?